2020’s smash hit documentary, Tiger King is not likely to age well. BUT, through the haze of dubious animal handling, aggressive and dangerous interpersonal conflict, and all-around disorienting approach to life and personal finances… there’s a conversation worth opening up about sexual health.
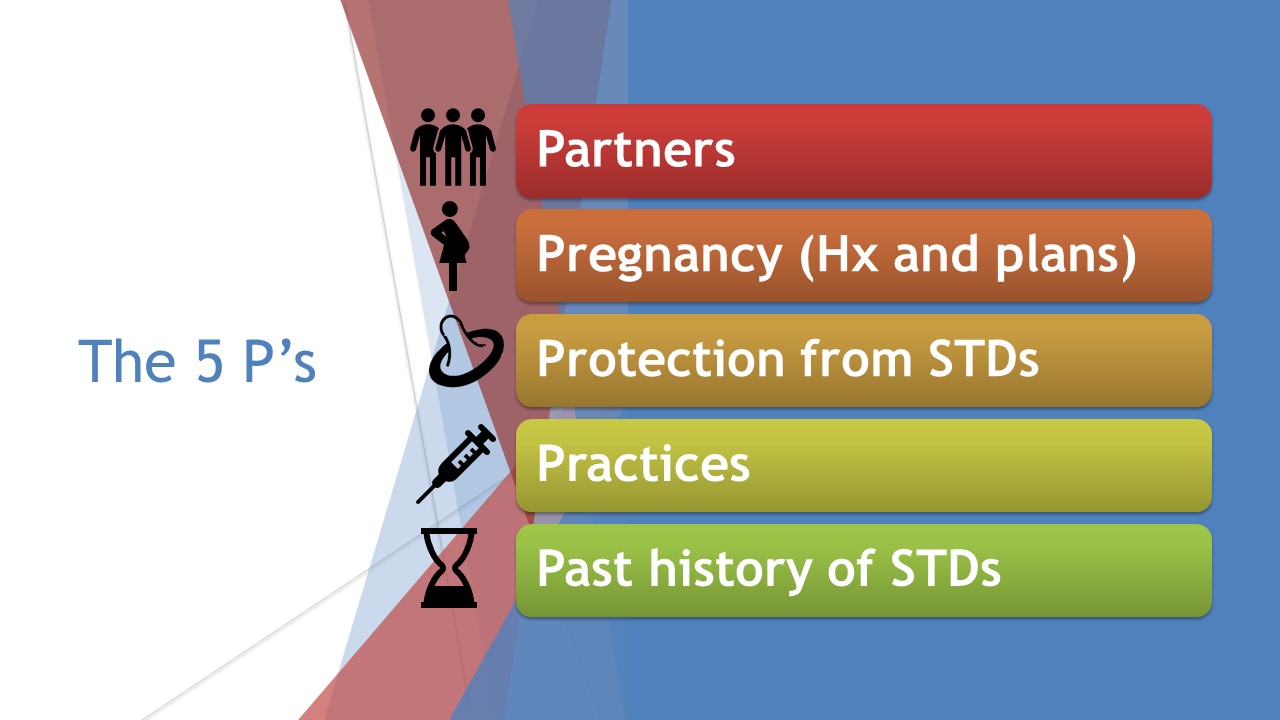
I’m using the CDC’s “5 P’s” method of taking a sexual history to examine missed opportunities and how we as providers can have better conversations with our patients.
In the second part of this investigation, let’s pick up where we left off, with…
#3 Pregnancy (Prevention or Plans)
Assumptions about pregnancy during a sexual history often revolve around age: this person is too young to want kids, or too young to know that they don’t. Certain pregnancies (read: married women in their late 20’s/early 30’s) are assumed to be good news when they could be emotionally or financially devastating. Some folks, especially transgender patients and queer couples, may be interested in building a family and feel discouraged that their provider assumes they won’t have kids.
It’s easy to say that John’s not a risk for pregnancy. As a cis man, he can’t get pregnant, and he probably doesn’t need to consider birth control if his primary partner is also a cis man. But we don’t know what John wants for his future: is he interested in having kids? Towards the end of Tiger King, John leaves Joe Exotic for a female coworker. He is now married to a woman and has a child. Were children always part of John’s plans? A good sexual history could have given a hint.

#4 Past History of STIs
Asking about previous STI infections is done primarily to assess for risk of a future STI. In John’s case, we know very little about his history before marrying Joe. We also don’t know if Joe or John might have contracted an STI from outside of their relationship. Understanding John’s past history of STIs can help provide guidance and education for prevention of a future STI.
Moreover, if John did have a previous STI, we want to know if and how it was treated. This is an important time to consider the health literacy of the patient. Does John know that he needs to take antibiotics for the full prescribed time, even if he feels better? Does he know that he can be a carrier for an infection even if he has no symptoms? Many people do not regularly get tested for STIs based on the misconception that they “don’t feel sick.” Talking about a history of STIs also means creating a plan for getting tested on a regular basis if appropriate.
#5 Prevention of STIs
Finally, preventing future STI infections requires education and a plan. Some patients simply don’t know that there are safer sex options out there besides external condoms. A good provider can teach patients about internal condoms, dental dams, gloves, and lube. But whether a patient will use any of these tools? That requires a deeper conversation.
For John, we might ask about his sexual identity. Throughout Tiger King, there are references to the fact that John identifies as straight. For some folks, when sexual identity and sexual behavior don’t line up, they also don’t use the same safer sex precautions. ((there is solid research to this phenomenon among lesbian women who do not use birth control with male partners as well)) Does John feel protection is necessary?
Moreover, we might need to ask, if John’s partner Joe allows him to use condoms or other safer sex tools? This is an example of reproductive coercion; abusive partners sometimes refuse the use of safer sex tools as a means of power over their partner. This could be another clue that John is in danger and needs access to supportive services beyond sexual healthcare.

An Extra P: PLEASURE
The CDC model doesn’t prioritize talking about sexual pleasure, but there is so much to be gained by including this topic in your sexual histories. Who knows if John was experiencing pleasure in his encounters with Joe? Did the pursuit of pleasure keep him in that relationship or push him away from it faster? How do we even ask those questions? You can learn more about how to talk about pleasure with your patients from a webinar I created, “Why Pleasure Matters,” which is available through the Intimate Health Consulting Store.
Thankfully, John Finlay has a new, and (hopefully) healthier life post-Tiger King. His sexual history today probably looks a lot different than it did in 2016. We take sexual histories yearly because our patients’ lives change rapidly and dramatically, and so do their sexual health needs. A sexual history has the ability to uncover so many things about a patient’s life… if you ask the right questions.




